How Can Diabetes Affect Eye Health?
Patients with diabetes are at an increased risk of developing eye diseases that can cause vision loss and blindness, such as diabetic retinopathy, cataracts and glaucoma. These and other serious conditions often develop without vision loss or pain, so significant damage may be done to the eyes by the time the patient notices any symptoms. For this reason, it is very important for diabetic patients to have their eyes examined once a year. Diagnosing and treating eye disease early can prevent vision loss. It is also important to maintain a steady blood-sugar level, take prescribed medications, follow a healthy diet, exercise regularly and avoid smoking.
How Is Diabetic Retinopathy Treated?
It is very important for diabetic patients to have their eyes examined once a year. Diagnosing and treating eye disease early can prevent vision loss. It is also important to maintain a steady blood-sugar level, take prescribed medications, follow a healthy diet, exercise regularly and avoid smoking.
What Happens If Diabetic Retinopathy Is Left Untreated?
If you opt to not see a doctor or medical professional for your diabetic retinopathy, you’re rolling the dice with your vision. This isn’t something to mess with.
In most cases, early nonproliferative retinopathy will progress to proliferative retinopathy if not treated. This will continue to worsen until the patient can become blind. If you have diabetes, managing your blood sugar levels can slow the progression, but it’s a dangerous line of thinking to hope this disease will go away without treatment. What will go away is your vision.
These are the complications of having diabetic retinopathy, all lead to serious vision damage:
- Vitreous hemorrhage — When the abnormal blood vessels bleed into the vitreous it may cause you to see a few dark spots if the bleeding is minimal. But if the bleeding becomes more severe the vitreous cavity can fill with blood and completely block your vision. Vitreous hemorrhage won’t cause permanent vision loss, as the blood can clear or be removed.
- Retinal detachment — The abnormal blood vessels formed stimulate the growth of scar tissue, which can pull the retina away from the back of the eye. In slight detachment, this will cause flashes of light and floaters. In severe detachment, vision loss can result.
- Glaucoma — As abnormal blood vessels grow, they can interfere with the normal flow of fluid through and out of the eye. This causes pressure to build in the eye, and this is glaucoma. If untreated, this pressure can eventually damage the optic nerve, permanently damaging vision.
- Blindness — Complete vision loss is the result of untreated diabetic retinopathy.
What People Say About Us!
LOVE this Eye group & staff. Being a medical professional for many years, I have interacted with a higher than average number of groups from the West coast to here, & this one is professional, polite & kind. The doctors are the best of the best in Opthalmology. So very thankful I found them.
Click here to read more reviews.
How Quickly Can Diabetic Retinopathy Progress?
Diabetic retinopathy can occur in patients with either type 1 or type 2 diabetes. Typically, diabetic patients will develop diabetic retinopathy after they have had diabetes for between 3 and 5 years. How quickly it progresses is dependent on many factors, such as how well the patient manages their blood sugar and what treatments they are receiving.
In the early stages, diabetic retinopathy will not affect your sight, but it will progress. That’s why it’s so important for patients with diabetes to have yearly eye exams to spot the condition before it starts impacting vision.
What Is The Progression Of Diabetic Retinopathy?
Basically, diabetic retinopathy can be broken down into two forms — nonproliferative and proliferative. The disease progresses through four stages:
- Mild nonproliferative retinopathy — Small areas of balloon-like swelling in the retina’s tiny blood vessels characterize this earliest stage. These “microaneurysms” may leak fluid into the retina, leading to the development of floaters. But this isn’t always the case. When they don’t, the patient has no symptoms.
- Moderate nonproliferative retinopathy — Now the blood vessels that nourish the retina may swell and distort. They may also lose their ability to transport blood. Both conditions cause characteristic changes in the appearance of the retina and will likely lead to diabetic macular edema, a build-up of fluid in the macula. The macula is the area of the retina used for sharp, straight-ahead vision.
- Severe nonproliferative retinopathy — As more and more blood vessels in the retina become blocked, blood is deprived to areas of the retina. These areas respond by secreting growth factors that signal the retina to grow new blood vessels.
- Proliferative diabetic retinopathy — The most advanced stage accelerates growth of abnormal new blood vessels. They now grow along the inside surface of the retina and into the vitreous gel that fills the interior of the eye. These abnormal vessels are weak/fragile, and they are likely to leak and bleed. Scar tissue that has formed as vessels become blocked can contract at this point and pull on the retina, causing retinal detachment. This is where the retina pulls away from the back of the eye, and it can lead to permanent vision loss.
Is There Any Pain With Diabetic Retinopathy?
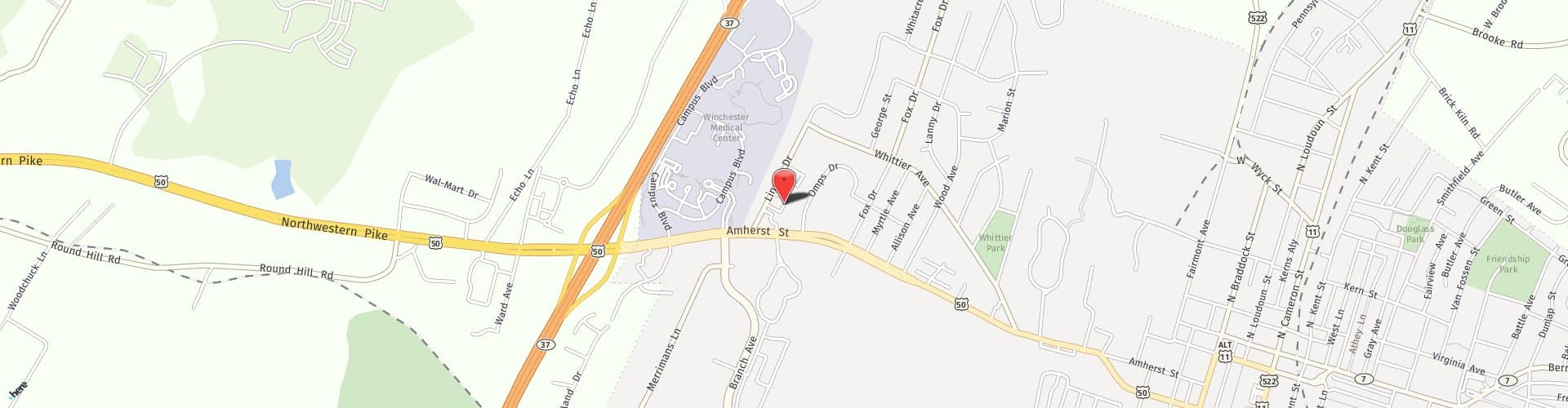
There isn’t any pain. That’s another problem, as the disease can progress unbeknownst to the person. Their vision may not have been substantially affected at this point and they don’t have any pain. Not to be crazy about this, but that’s why patients with diabetes need to come see us at Shenandoah yearly for an eye exam.
Is There Recovery After Treatment For Diabetic Retinopathy?
Early treatments may be nothing more than managing your blood sugar effectively. Newer treatments use anti-VEGF injections to stem the growth of abnormal blood vessels. Recovery is minimal. Focal and scatter laser treatments can make your vision blurry for a day or so afterwards, but that’s about it. Vitrectomy, where blood is removed from the middle of the eye, is more involved and will involve some recovery.